Meet Lenacapavir, an HIV Prevention Injection, Price and its Mechanism.
Besides other HIV prevention measures like the use of prevention PREP for Truvada, PEP and others there's a new development, yet to be introduced in Uganda. The Lenacapavir HIV Prevention Injection that is given twice a year, every six months. So far tested in women at high of acquiring HIV and proven effective.
It is really good news towards the development for the research of HIV prevention drugs, but it may be impossible or a few people may be able to access it in Uganda, due to its monetary value attached, for example it is approximately 40.000 USD in the USA, which is equivalent to One Hundred forty six million, three hundred eighteen thousand, eight hundred forty seven , (146,318,847) Ugx.
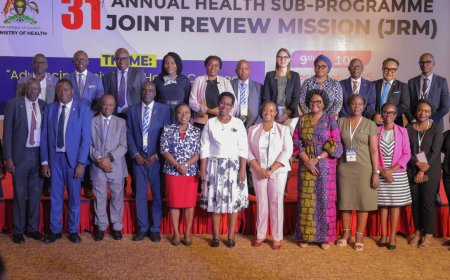
But the good news is, if the demand for it is high in Uganda, there could be chances for a reduced price tagged for this injection. Dr. Flavia Matovu Kiweewa, the lead researcher with the Makerere University Johns Hopkins University (MUJHU) explained this to journalists during a Media Cafe organized by health journalists through their network of Health Journalist Network Uganda ( HEJNU), at their headquarters in Kampala.
On Friday, she said that so far the trials which have been done in Uganda and South Africa indicate hope that Lenacapavir can effectively curb the spread of HIV in the two groups of people, the adolescents and young women .
Dr. Kiweewa, while explaining about the effectiveness and its mechanism, she said Lenacapavir Injection is long-acting formulation that lasts six months. The injection forms a depot under the skin, releasing the drug slowly over time, requiring re-injection every six months as compared to other long-acting formulations like cabotegravir, which only last for two months.
On its efficacy results and Implications, Dr. Kiweewa mentioned that zero HIV infections occurred in the injection group, translating to 100% protection and its results were presented in Munich, receiving widespread acclaim for the unprecedented efficacy.
She added that with other HIV prevention methods, there is a lack of 100% efficacy, for example in previous interventions. The conducted study also assessed the performance of FTA and TDF against each other, showing mixed results due to adherence issues.

Discussing the challenges, she described that of adherence, where many participants did not take their drugs as instructed. The study found that non-adherence is a significant factor in HIV infections, with non-adherent participants having minimal drug levels in their bodies, but the study also examined pregnancy outcomes, with over 500 pregnancies recorded, mostly in Uganda.
The injection was shown to be safe in pregnant women, offering potential protection for both the mother and the infant. Therefore the plans for making the injection accessible, including filing for licensure with the FDA, the process involves inspections and audits to ensure the study was conducted ethically and according to good clinical practice, said Kiweewa
The goal is to have the injection approved for use in public facilities by 2025, with generics being produced to make it more affordable. The study also included results from Purpose 2, which looked at the injection in men who have sex with men and transgender women, showing consistent results.
She, however, emphasized the importance of making the injection accessible to the populations that need it with plans to produce generics at a lower cost to make the drug affordable for resource-limited countries. The voluntary licensing agreements with generic manufacturers to ensure the drug is available at a lower cost should be considered, said Dr. Kiweewa.
"The goal is to have the injection available in the next two years, with participants in the study receiving access before full implementation, the next steps are to make the injection accessible. The study has shown promising results, and the focus is now on ensuring the drug is available to those who need it. But the process involves multiple steps, including FDA approval, local authority approval, and generic manufacturing but the main goal is to ensure availability of the drug in public facilities by 2025."
Dr. Steven Asiimwe, Prevention officer and Researcher with the Uganda Aids Commission noted how their approach to prevention is a combination because one intervention may not be enough.
The combination approach has different things like biomedical intervention, PREP, PEP, and the ABC method. Other interventions include working at the structural level , dealing with stigma , to reduce discrimination against people with HIV, he said
“As opposed to a licence, the Uganda Aids Commission wants to act more to ensure the drug is available, but it begins with evidence to prove that something works. Once the evidence about an intervention is presented and accumulated to the government , it is then good to proceed to the next step of the regulation, which is the second limitation or barrier.”
Dr. Asiimwe also highlighted that because many of these studies are international, they need to get approval from the FDA, but in Uganda it is the NDA that approves. That means the Lenacapavir intervention passed beyond the two barriers of evidence and regulations, then it the cost issue that comes as a barrier. However, as Uganda Aids Commission thinks about cost it also considers other options. Lenacapavir is still at the licensing level now but all those intervention are seen as the expanding options, he addressed.